Find below a selection of research results from the projects on data from SNAC-K.
Monitoring older adults’ health for preventive and early interventions: validation of the Health Assessment Tool (HAT)
The early identification of health declines in older primary care patients is essential to implement interventions for maintaining physical and mental capacity and function. The recent COVID-19 pandemic has stressed the lack of available comprehensive health measures that could help in assessing risk, prioritizing hospitalization and planning vaccination. Our group has developed the Health Assessment Tool (HAT) and its derived sex-specific geriatric health charts to measure the dynamic and heterogeneous health status of older populations, based on data from the Swedish National Study on Aging and Care in Kungsholmen (SNAC-K). Still, the validity and feasibility of HAT in clinical practice has not been tested. In the context of this project, we are examining: 1) the external validity of HAT in different Swedish population-based cohort studies; 2) the reliability and prognostic value of HAT in the primary care setting; and 3) the feasibility and acceptability of using HAT in primary care.
Aim 1 has already been executed (paper submitted) using data from the three other cohorts belonging to the Swedish National study on Aging and Care (SNAC). We showed that HAT is a highly predictive, clinically intuitive, and externally valid health assessment tool with potential for better addressing older adults’ care needs individually and optimizing risk stratification at the population level.
Aims 2 and 3 are ongoing. Data on more than 800 patients has been collected 2023 across six urban, rural and semi-rural primary care centers in Sweden. Moreover, we have carried out four individual Interviews with primary care coordinators (verksamhetschef), one focus group with the data collection team, and 8 individual interviews with patients to investigate the acceptability and usability of the tool. Our final goal is to support primary care professionals in planning personalized interventions to preserve older adults’ health. (Calderón-Larrañaga A et al. Submitted, 2024)
15-year transitions across living and care settings in a population of Swedish older adults
Older individuals with complex health profiles and poor social support are often exposed to frequent and recurrent transitions across different living and care settings. It has been shown that fragmented care is a risk factor for unavoidable hospitalizations, increased mortality, and healthcare expenditure. Poor treatment adherence and accelerated functional decline can be further consequences of frequent and recurrent care transitions, with a strong impact on older adults’ quality of life. Consequently, timely identification of older individuals at higher risk of excessive frequent care transitions is of utmost importance for effective and efficient transitional care. Taking advantage of the longitudinal data from the Swedish National Study on Aging and Care in Kungsholmen (SNAC-K), this study (under preparation) aims to investigate the association of sociodemographic, clinical, and functional characteristics with; 1) the volume of transitions across living and care settings; and 2) specific trajectories across living and care settings (home, home care, nursing home, and hospital).
Results indicate that over 15 years, the average length of stay was two years at home without formal social care, one year with formal social care, one year in a nursing home, eight days in a hospital, and 17 days in post-acute care. After hospital discharge, older age and being a woman increased the chance of receiving home social care. Multimorbidity and slow walking speed were associated with a higher risk of hospitalization and formal home care after discharge. Cognitive impairment raised the risk of institutionalization. Disability was associated with a higher risk of nursing home placement after hospital discharge.
In conclusion, different sociodemographic, clinical, and functional characteristics are associated with specific care transition patterns, emphasizing the importance of identifying older adults at risk for frequent care transitions on time to improve transitional care efficiency and effectiveness. (Gentili S & Vetrano D. Work in progress, 2024)
Association of white matter hyperintensity accumulation with domain-specific cognitive decline: a population-based cohort study
We investigated the association of load and accumulation of white matter hyperintensities (WMHs) with rate of cognitive decline. This population-based study included 510 dementia-free people (age ≥60 years) who had repeated measures of global and regional (lobar, deep, periventricular) WMHs up to 6 years (from 2001–2003 to 2007–2010) and repeated measures of cognitive function (episodic memory, semantic memory, category fluency, letter fluency, executive function, perceptual speed) up to 15 years (from 2001–2004 to 2016–2019). We found that greater baseline loads of global and regional WMHs were associated with faster decline in letter fluency, perceptual speed, and global cognition. Furthermore, faster accumulation of global, deep, and periventricular WMHs was related to accelerated cognitive decline, primarily in perceptual speed. These data show that WMHs are associated with decline in perceptual speed rather than episodic or semantic memory and that cognitive change is more vulnerable to WMH accumulations in deep and periventricular regions. (Li Y, et al. Neurobiology of Aging 2023)
Slow walking speed improved the detection of prodromal dementia
Cognitive impairment, no dementia (CIND) is considered an at-risk condition for dementia. However, many older individuals with CIND will remain cognitively stable or even revert to a normal state of cognition. In this study, we investigated whether adding a test of motor function (i.e. walking speed) to the neuropsychological assessment improves our ability to detect dementia. Using data spanning over 12 years of follow-up we found that people with co-occurring cognitive and motor dysfunction experience the highest risk of dementia. Also, adding an easy‐to‐perform measurement of physical function—such as walking speed—to a standard cognitive battery dramatically improved the detection of prodromal dementia. Taken together, these findings point toward a strong relationship between cognitive and physical domains in the development of dementia, suggesting that markers of both may help in a better dementia risk assessment (Grande, et al. Alzheimers Dement 2020)
Genetic risk of dementia is mitigated by cognitive reserve
We investigated if lifelong engagement in activities promoting cognitive reserve (eg. early life education, midlife substantive work complexity, late life leisure activities and social networks) modified the risk of dementia attributable to Apolipoprotein ε4 allele (APOE‐ε4), a well‐known genetic risk factor for dementia. Using 9-year follow-up data on 2,556 SNAC-K participants, we found that relative to APOE‐ε4 carriers with low cognitive reserve, ε4 carriers with high reserve experienced dementia risk reduction equivalent to ε4 noncarriers with high reserve. These results indicate that lifelong engagement in reserve‐enhancing activities attenuates the risk of dementia attributable to APOE‐ε4. Importantly, these findings suggest that promoting cognitive reserve might be especially effective in subpopulations with high genetic risk of dementia (Dekhtyar et al., Annals of Neurology 2019).
Participating in Mental, Social, and Physical Leisure Activities and Having a Rich Social Network Reduces the Incidence of Diabetes-Related Dementia in Older Adults
In this study, we investigated whether greater engagement in leisure activities and a richer social network may compensate for the increased risk of dementia in older adults with diabetes. During 10-year follow-up, diabetes was associated with a 2-times greater risk of dementia, especially of vascular origin. However, this increased dementia risk appeared to be mitigated by active engagement in leisure activities or a rich social network. We estimated that if all older adults with diabetes in our cohort had an active lifestyle, 48% of diabetes-related dementia cases could be prevented. These findings highlight that an active and socially integrated lifestyle could represent a key preventive strategy for dementia, especially in high-risk people, such as those affected by diabetes (Marseglia et al., Diabetes Care 2019).
Neuropsychiatric multimorbidity strongly affect physical function
During a 9-year follow-up, SNAC-K participants with multiple cardiovascular and neuropsychiatric diseases showed the greatest declines in walking speed and in the ability of perform several activities of daily living. In particular, a significant decline over time for both walking speed and disability was observed in people with one or more neuropsychiatric diseases, but only for walking speed in those with cardiovascular multimorbidity. Multiple neuropsychiatric diseases may play a greater role in functional decline in older people than multiple cardiovascular diseases. Both patients and physicians should be aware that neuropsychiatric diseases are major predisposing factors for functional decline (Vetrano DL et al, Plos Medicine 2018)
Atrial fibrillation, antithrombotic treatment, and cognitive aging
In this population-based cohort study of people aged 60 years and older, atrial fibrillation (AF) was associated with faster cognitive decline and a higher risk of dementia, independent of clinical stroke. Among participants with AF, use of anticoagulants was associated with a lower risk of dementia, suggesting potential cognitive benefits of anticoagulant therapy in patients with AF (Ding M et al, Neurology 2018).
Geriatric health charts for individual assessment and prediction of care needs
The Health Assessment Tool (HAT) is a composite measure that summarizes the information provided by five health indicators commonly available in various health settings: severe and mild disability, cognitive and physical functioning and multimorbidity. Geriatric health charts built based on HAT scores can help care providers interpret individual scores in the context of a reference population of the same age and sex. The charts can be used to forecast future trajectories of health and care needs both at the individual (e.g. planning of home care) and population (e.g. resource allocation) levels. Individual-level HAT scores and the corresponding provisory health curves can be obtained using the online calculator at the following link: HAT-calculator for people 60 years and older (Santoni G et al, J Gerontol A Biol Sci Med Sci 2016 & 2018, JAMDA 2018).
Lifestyle behaviors and longevity
Maintaining a healthy lifestyle and a rich social networkwas positively associated with survival even among people aged 75 years and older. People who reported being physically active lived 2 years longer than those who did not. Nonsmokers who were physically and mentally active and had a good social network (low risk profile) lived about 5 years longer than those who smoked, were inactive, and had a poor social network (high risk profile). These associations were also found in individuals aged 85 years and older and those with chronic diseases (Rizzuto et al, BMJ 2012).
Genetic influences in aging
Recently, researchers have suggested that there is a relationship between telomere length and longevity such that longer telomeres are associated with an increased life span. We have examined the role of a gene (hTERT) that is involved in the modulation of the human telomerase on longevity in 2 cohorts of older adults—Kungsholmen project and SNAC-K. We found an association between the -1327T/C polymorphism of the hTERT gene and survival in women aged 75+. Female T/T carriers lived 2-3 years longer than the C/C carriers. This effect was not present in men or in younger people aged 60–72 years (Kalpouzos G et al., J Gerontol A Biol Sci Med Sci 2014).
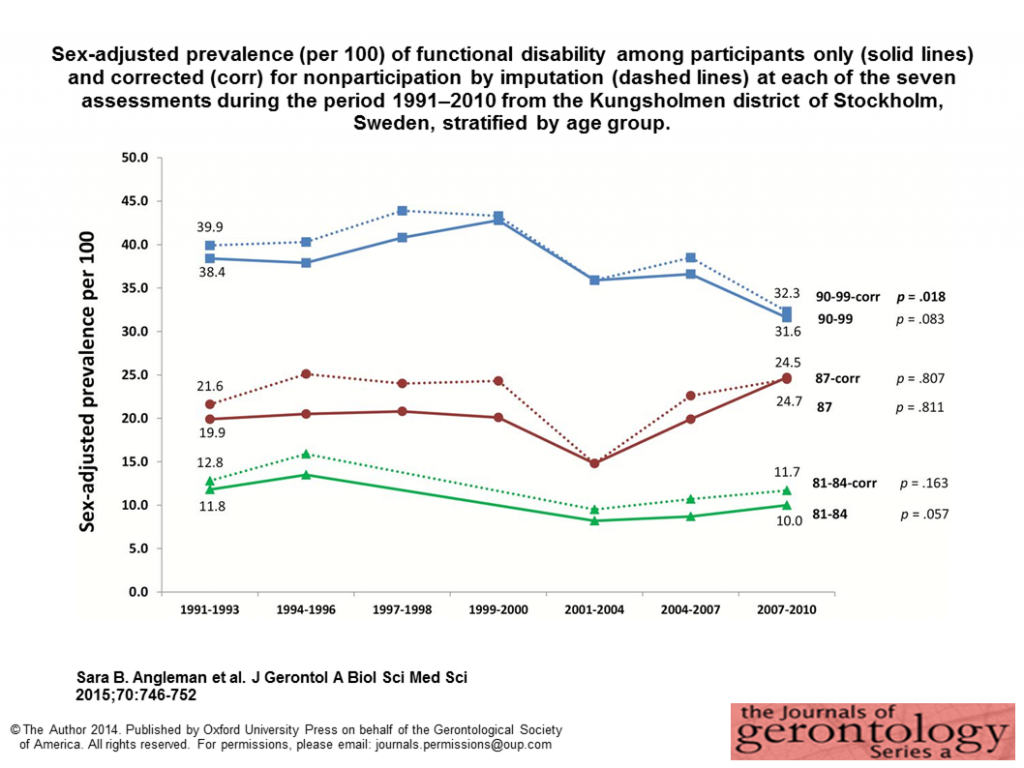
Temporal trends in functional dependence and survival
We compared prevalence, incidence, and mortality associated with ADL disability during the 1990s and 2000s. Both prevalence and incidence of disability remained stable during the last decades in this urban Swedish population, with a trend towards a slow decline. Mortality remained steady among disabled persons but decreased among persons without disability, suggesting that increased life expectancy in the last decades may be essentially driven by longer lives of functionally independent people (Angleman et al, J Gerontol A Biol Sci Med Sci 2014).
Cognition and brain aging
Exploring the individual differences in cognitive changes in healthy aging, we found that age differences in cognitive performance at baseline in SNAC-K are most pronounced for processing speed and episodic memory performance. In addition, single genetic polymorphisms can only explain small portions of the individual differences in these cognitive abilities in old age (Laukka et al, Psychol Aging 2013).
Mental disorders in aging
Moderate/severe unipolar depression was associated with poorer performance on several cognitive tasks, whereas mild depression was associated only with poorer performance in processing speed. No association between depression and short-term memory, general knowledge, or spatial ability was observed. Increasing age, use of pharmacological treatments that may affect cognitive performance, and incipient dementia did not exacerbate the depression-related cognitive deficits (Pantzar et al, Psychol Med 2013).
The effect of diabetes on aging
Genetic association studies suggest that variation in the HHEX–IDE gene region may underlie the relationship between diabetes and dementia. In collaboration with the department of Medical Epidemiology and Biostatistics (MEB), KI, we tested this hypothesis in 2 cohorts of elderly people (Kungsholmen Project and SNAC-K) and found that in both cohorts, the AA genotype interacts with diabetes to multiply the risk of dementia and AD among elderly Swedish people (Xu et al, accepted in PLOS Medicine). Vascular burden undermines brain integrity. In our exploration of the factors that contribute to loss of brain integrity in aging, we found that old age, genetic susceptibility (e.g. APOE ε4), and increased burden of vascular risk factors (e.g. hypertension, diabetes) are associated with brain pathology. Specifically, we showed that the aggregation of heavy alcohol consumption, hypertension, diabetes, and current smoking is detrimental to white-matter integrity, and that this effect is more pronounced among APOE ε4 carriers (Wang et al, Neurology 2015).
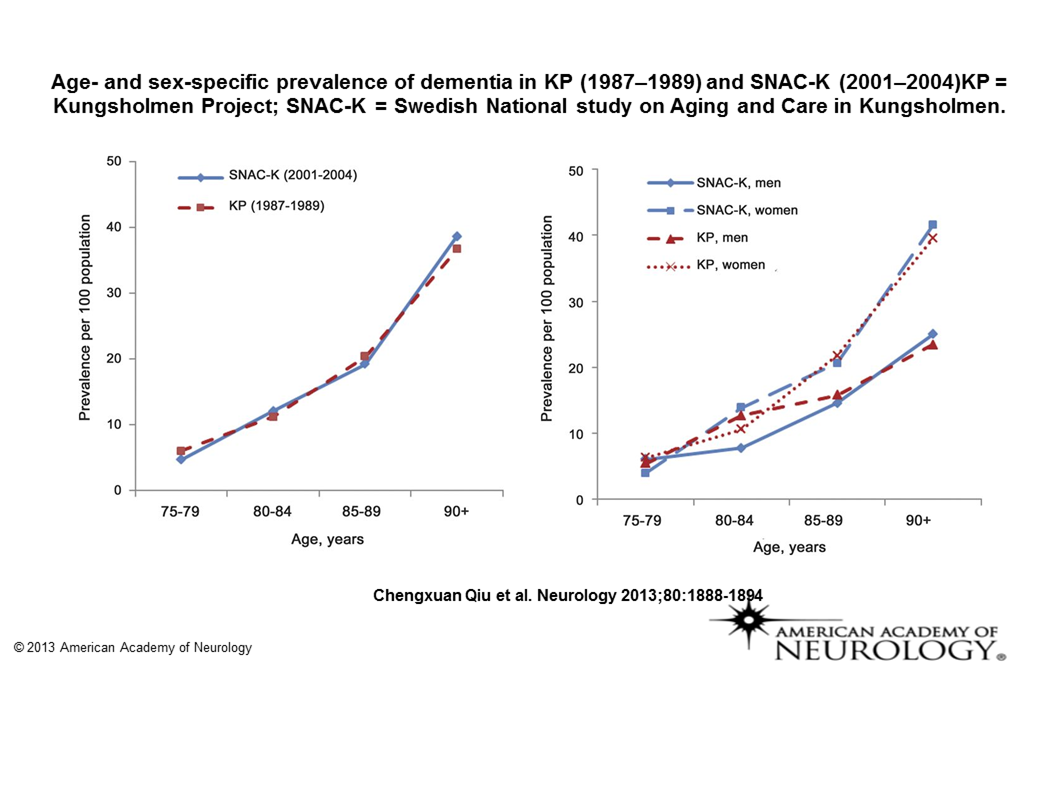
Secular trends in dementia occurrence from the 1980s through the 2000s
Data from the Kungsholmen Project and the SNAC-K study showed that the prevalence of dementia was stable between 1987−89 and 2001−04 in central Stockholm, Sweden, whereas the survival of patients with dementia increased. These results suggest that incidence of dementia may have decreased over the last 2 decades in this region (Qiu et al, Neurology 2013).
Effect of negative life events on brain volume
Previous research suggested that psychosocial stress exacerbates the risk for dementia, but because of variations in stress measures and study populations, the results of earlier studies have been inconsistent. In collaboration with the department of MEB, KI, we examined the relationship between negative events experienced throughout the entire lifespan and hippocampal and amygdala volumes in older adults. The results suggest that the effect of negative life events on the brain depends on the time when the events occurred, with the strongest effects observed during the critical time periods of early and late life (Gerritsen et al, Psychol Med 2014).
Air pollution and mortality
In the multicenter European Study of Cohorts for Air Pollution Effects (ESCAPE), researchers investigated the association between natural-cause mortality and long-term exposure to several air pollutants. Data from 22 European cohort studies created a total study population of 367,251. The findings support the hypothesis that there is an association between long-term exposure to ambient particulate matter air pollution and mortality, even at concentrations below the existing European Union limit values (Beelen et al., Lancet 2014).
